Bimonthly exam for the month of December 2020
1) A 55 year old man with Recurrent Focal Seizures
Detailed patient case report here: http://ushaindurthi.
1. What is the problem representation of this patient and what could be the anatomical site of lesion ?
55 year old man presented with the right upper limb weakness and focal seizures involving right upper limb and lower limb.
The anatomical site of lesion could be:
1.Left Frontal lobe infarct - Present as Seizures are typically brief, and can have prominent vocalization, bizarre behavior, urinary incontinence, and head and eye deviatiation
2.Left Parietal infarct - Primary sensory area (post-central gyrus)
3.Seizures onset with contralateral (or rarely ipsilateral or bilateral) focal somatosensory seizure, most commonly paraesthesias with tingling and/or numbness.
Non-dominant parietal region: Spatial disorientation
4.Left Temporal infarct - Temporal lobe seizures are characterized by behavioral arrest and impaired awareness. It is usually preceeded by aura. Aura could be sensory, emotional, cognitive, or autonomic features prior to onset of impaired awareness. Postictal confusion typically occurs.
5.Left Occipital infarct - Visual hallucinations are the hallmark of occipital seizures, but are not invariably present. Hallucinations typically commence in the visual field contralateral to the affected visual cortex and then spread to involve the entire visual field
6.Left Internal capsule infarct - Classic lacunar strokes syndrome that arises from lesions of the internal capsule are pure motor strokes, ataxic hemiparesis, and clumsy hand-dysarthria.
https://www.epilepsydiagnosis.org/seizure/frontal-lobe-overview.html
2. Why are subcortical internal capsular infarcts more common that cortical infarcts?
Cerebrovascular accidents are more common in subcortical areas because the perforating arteries that supply the region are predisposed to occlusion or rupture due to their small diameter.
Ischemic strokes secondary to blockage of the perforating arteries are known as lacunar strokes.
The mechanisms of lacunar strokes include
1. Lipohyalinosis of perforating blood vessels - Most common cause
2. Atherosclerosis of the large trunk vessels that supply perforators
3. Embolic occlusion of the perforating arteries.
https://www.ncbi.nlm.nih.gov/books/NBK542181/
3. What is the pathogenesis involved in cerebral infarct related seizures?
Seizure initiation is characterized by two concurrent events:
1) high-frequency bursts of action potentials, and
2) hypersynchronization of a neuronal population.
Sustained neuronal depolarization resulting in a burst of action potentials, a plateau-like depolarization associated with completion of the action potential burst, and then a rapid repolarization followed by hyperpolarization.
The bursting activity resulting from the relatively prolonged depolarization of the neuronal membrane is due to influx of extracellular Ca++, which leads to the opening of voltage-dependent Na+ channels, influx of Na+, and generation of repetitive action potentials. The subsequent hyperpolarizing afterpotential is mediated by GABA receptors and Cl− influx, or by K+ efflux,
Seizure propagation, the process by which a partial seizure spreads within the brain, occurs when there is sufficient activation to recruit surrounding neurons.
This leads to a loss of surround inhibition and spread of seizure activity into contiguous areas via local cortical connections, and to more distant areas via long association pathways such as the corpus callosum.
The propagation of bursting activity is normally prevented by intact hyperpolarization and a region of surrounding inhibition created by inhibitory neurons. With sufficient activation there is a recruitment of surrounding neurons via a number of mechanisms. Repetitive discharges lead to: 1) an increase in extracellular K+, which blunts the extent of hyperpolarizing outward K+ currents, tending to depolarize neighboring neurons; 2) accumulation of Ca++ in presynaptic terminals, leading to enhanced neurotransmitter release; and 3) depolarization-induced activation of the NMDA subtype of the excitatory amino acid receptor, which causes more Ca++ influx and neuronal activation.
https://www.ncbi.nlm.nih.gov/books/NBK2510/
https://www.pharmatutor.org/articles/epilepsy-brief-review
4. What is your take on the ecg?
ECG shows Sinus Rhythm with LAD, Left Anterior Fasciular Block with VPCS and
NSTEMI in septal leads ( seen on the day of admission -28/11/2020 and in anteroseptal leads on 30/11/2020)
CRITERIA FOR LAFB IN ECG:
Left axis deviation (usually between -45 and -90 degrees)Small Q waves with tall R waves (= ‘qR complexes’) in leads I and aVLSmall R waves with deep S waves (= ‘rS complexes’) in leads II, III, aVF
https://litfl.com/left-anterior-fascicular-block-lafb-ecg-library/
And do you agree with the treating team on starting the patient on Enoxaparin?
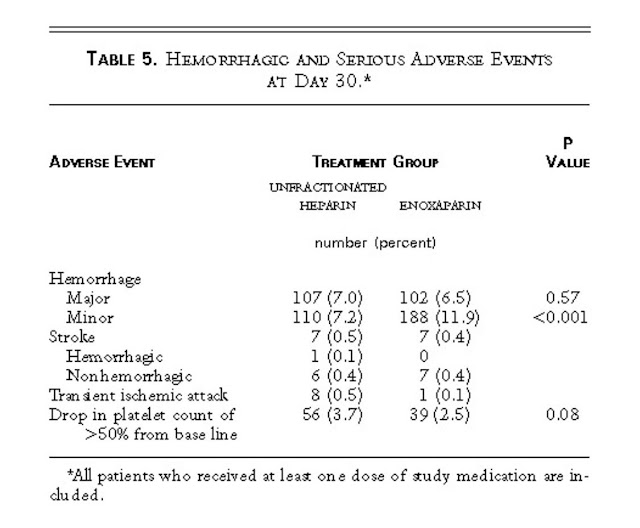
A Comparison of Low-Molecular-Weight Heparin with Unfractionated Heparin for Unstable Coronary Artery Disease
P - 3171 patients with angina at rest or non–Q-wave myocardial infarction were included in a double-blind, placebo-controlled study
I - 1 mg of enoxaparin (low-molecular-weight heparin) per kilogram of body weight, administered subcutaneously twice daily
C - Continuous intravenous unfractionated heparin
Therapy was continued for a minimum of 48 hours to a maximum of 8 days, and we collected data on important coronary end points over a period of 30 days.
O -
At 14 days the risk of death, myocardial infarction, or recurrent angina was significantly lower in the patients assigned to enoxaparin than in those assigned to unfractionated heparin (16.6 percent vs. 19.8 percent, P = 0.019).
At 30 days, the risk of this composite end point remained significantly lower in the enoxaparin group (19.8 percent vs. 23.3 percent, P = 0.016). The need for revascularization procedures at 30 days was also significantly less frequent in the patients assigned to enoxaparin (27.0 percent vs. 32.2 percent, P = 0.001).
The 30-day incidence of major bleeding complications was 6.5 percent in the enoxaparin group and 7.0 percent in the unfractionated-heparin group but the incidence of bleeding overall was significantly higher in the enoxaparin group (18.4 percent vs. 14.2 percent, P = 0.001), primarily because of ecchymoses at injection sites.
https://www.nejm.org/doi/full/10.1056/NEJM199708143370702
5. Which AED would you prefer?
If so why?
Please provide studies on efficacies of each of the treatment given to this patient.
https://www.e-sciencecentral.org/upload/er/thumb/er-4-2-39f2.gif
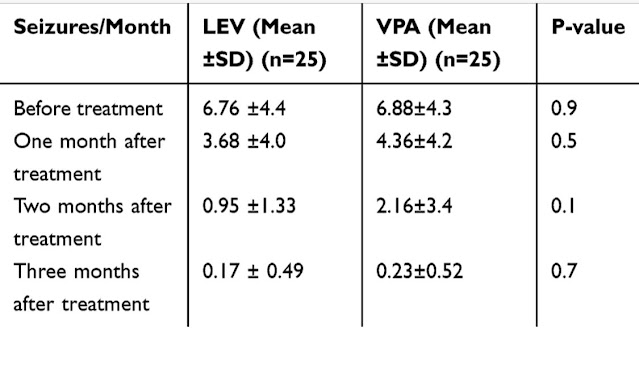
This study compared the effect of levetiracetam (LEV) as monotherapy to sodium valproate (VPA) as monotherapy on cognitive functions in patients with epilepsy.
P -This was a comparative prospective study on 50 patients with newly diagnosed epilepsy started on antiseizure medications.
I - 25 patients received Levipil
C - 25 other patients received Sodium valproate
O -
Comparison of simple reaction–time test-score changes between groups revealed there was deterioration in scores in the VPA group compared to scores in the LEV group, which showed improvements in scores. There was a significant difference between groups 3 months after treatment, where means were 592.7±238.3 for LEV and 927.1±322.2 for VPA (p=0.005)
Comparison of choice reaction–time test-score changes between groups revealed deterioration in the scores in the VPA group compared to scores in the LEV group, which showed improvements.
Comparison of trail-making test A–score changes between groups revealed there was deterioration in scores in patients of group VPA compared to patients of group LEV, which showed improvement.
Comparison of trail-making test B–score changes between groups revealed there was deterioration in scores in patients of group VPA compared to group LEV, which showed improvements.
Comparison of WCST score changes in between groups revealed there was deterioration in WCST scores in patients of group VPA compared to group LEV, which showed improvements in scores. At 3 months after treatment, means were 44.04±4.7 for LEV and 25.08±5.33 for VPA (p˂0.0001), and significant improvement was seen from 32.68±5.8 pretreatment to 44.04±4.7 at 3 months after treatment in the LEV group (p˂0.0001)
Question 2) 55 year old man with Recurrent hypoglycemia
1. What is the problem representation for this patient?
55 year old man, known case of hypertension and Diabetic type 2 since 10 years with metabolic syndrome
Presented with
Dyspnea on exertion since 3 days
Dry cough since 3 days
Giddiness associated with profuse sweating
2. What is the cause for his recurrent hypoglycemia? And how would you evaluate?
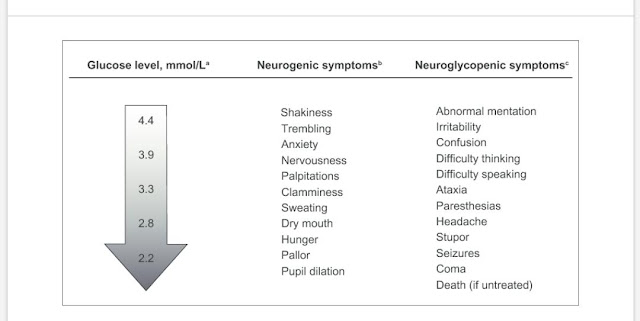
Some features Hypoglycemic patients could present to us with 👇
Here are some of the causes for Hypoglycemia 👇
From Harrisons Principles of Internal Medicine
2. What is the cause for his recurrent hypoglycemia? And how would you evaluate?
From the reports, he has elevated Serum Creatinine and Significant loss of proteins in his urine signifying a Renal Failure. Apart from that the patient is on OHA's - Glimiperide which is known to cause hypoglycemia.
Patients with decreased GFR due to diabetes and CKD have decreased insulin requirement as insulin is cleared by kidneys.
• In CKD patients the peripheral metabolism of insulin is reduced.
• With decrease in glycogen storage in the patients with CKD and uremia due to suboptimal nutrition anorexia may occur.
• There occurs less renal gluconeogenesis as a result of reduction in renal mass in CKD patients
Most of the medications used for treating diabetes are excreted by kidneys from the body. In CKD incidence of hypoglycaemia increases as a result of accumulation of these drugs and their metabolites.
https://www.peertechz.com/articles/doi10.17352-acn.000026.php
Population based cohort study to determine the association between use of sulphonylureas and risk of hypoglycaemia in relation to renal function and sulphonylurea metabolic group compared with use of metformin.
P- '120 803 new users of a non-insulin antidiabetic agent with at least one prescription and aged 18 years or more. The first prescription defined start of follow-up. Patients were followed until the end of data collection, a record for hypoglycaemia, or a blood glucose level of less than 3.0 mmol/L.'
Results - 'The risk of hypoglycaemia in current users of sulphonylureas only was significantly increased compared with current users of metformin only (adjusted hazard ratio 2.50, 95% confidence interval 2.23 to 2.82).
The higher risk in current users of sulphonylureas only was further increased in patients with an estimated glomerular filtration rate of less than 30 mL/min/1.73 m2 (4.96, 3.76 to 6.55). The risk of hypoglycaemia was also significantly higher in patients with a high sulphonylurea dose (3.12, 2.68 to 3.62) and in current users of glibenclamide (7.48, 4.89 to 11.44). Gliclazide, the sulphonylurea of first choice, showed a similar risk of hypoglycaemia compared with other sulphonylureas.'
'Sulphonylurea treatment in patients with a renal function of less than 30 mL/min/1.73 m2 should be considered with caution. Moreover, an increased risk of hypoglycaemic events was observed among all users of sulphonylureas.'
This study suggests that the risk of hypoglycaemia is significantly increased in current users of sulphonylureas only with severe renal impairment compared with users of metformin only
https://www.bmj.com/content/354/bmj.i3625
3. What is the cause for his Dyspnea? What is the reason for his albumin loss?
His chest Xray PA shows cardiomegaly with right pulmonary artery prominence with ? Pleural effusion probably secondary to Hypoalbuminemia and right sided consolidatory changes.
As the patient has been complaining of Dyspnea along with non productive dry cough the cause is probably due to Respiratory tract infection but i would also like to have a look at the patients 2Decho.
Albumin loss - Is clearly explained by the renal failure in this patient - with the significant spot pc ratio 3.91 and high serum creatinine 2.7mg/dl.
4. What is the pathogenesis involved in hypoglycemia ?
Counter-regulatory mechanisms include an interplay of hormones and neural signals to regulate the release of endogenous insulin, to increase hepatic glucose output, and to alter peripheral glucose utilization.
First line of defense against hypoglycemia - Among the counter-regulatory mechanisms, the regulation of insulin production plays a major role. Decreases in insulin production as a response to low serum glucose is the bodies first line of defense against hypoglycemia.
For endogenous glucose production to take place, particularly hepatic glycogenolysis, low insulin levels are necessary. As plasma glucose levels decline, beta cell secretion of insulin also decreases, thus leading to increased hepatic/renal gluconeogenesis and hepatic glycogenolysis. Glycogenolysis maintains serum glucose levels over 8 to 12 hours until glycogen stores are depleted. Over time, hepatic gluconeogenesis contributes more to maintaining euglycemia when required.
Additional counter regulatory mechanisms - Pancreatic alpha cells secrete Glucagon is the next line of defense against hypoglycemia.
Next line of counter regulatory mechanism- Adrenomedullary epinephrine is secreted.
Next line - Both release of growth hormone and cortisol are seen in prolonged hypoglycemia for more than 4 hours.
From Harrisons Principles of Internal Medicine
5. Do you agree with the treating team on starting the patient on antibiotics?
No, i do not agree with the treating team on starting the patient on antibiotics as he has no signs of sepsis.
A. 41 year old man with Polyarthralgia
Case details here: https://
1. How would you evaluate further this patient with Polyarthralgia?
From Harrisons Principles of Internal Medicine
From Harrisons Principles of Internal Medicine
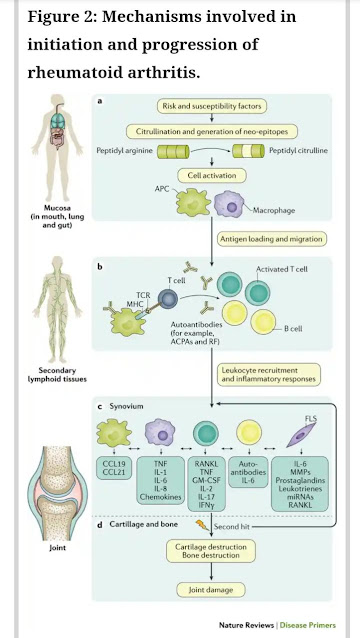
2. What is the pathogenesis involved in RA?
Post translation modifications such as citrullination or carbamylation in the mucosa -------> leads to neo-epitopes -------> Recognized by adaptive immune system ---------> These altered peptides are presented to Antigen presenting cells --------> Activating adaptive immune response -------> Activation of autoantibodies.
Stromal cells , APCs and macrophages can be activated locally --------> produce a range of inflammatory factors ---------> triggers synovial inflammation but may require a second hit, such as immune complex formation and complement activation ---------> induces cytokine production and synovial vascular leakage.
Paracrine and autocrine actions of cytokines, along with persistent adaptive immune responses, can perpetuate the disease and ultimately lead to cartilage and bone destruction.
3. What are the treatment regimens for a patient with RA and their efficacies
The current treatment strategy for RA involves a treat-to-target approach based on tight monitoring of disease activity and change of management if a treatment target is not reached.
Standard recommendations suggest Methotrexate plus short-term glucocorticoids. Methotrexate should be rapidly escalated to the optimal dose (25 mg once weekly) with folate substitution to mitigate or prevent adverse events without interfering with effectiveness.
Of note, in contrast to the anti-proliferative effects of methotrexate, which occur at much higher doses than used in RA, the anti-inflammatory effects of methotrexate do not involve the folate pathways.
Glucocorticoids should be given at a low dose or intermediate dose for a few weeks to a maximum of 4–5 months, when methotrexate (or another conventional synthetic DMARD) should have reached full effectiveness.
https://www.nature.com/articles/nrdp20181
TNF inhibitors, IL-6 receptor inhibitors and JAK inhibitors block the action of the pro-inflammatory cytokines involved in the initiation and progression of rheumatoid arthritis (RA)
A.
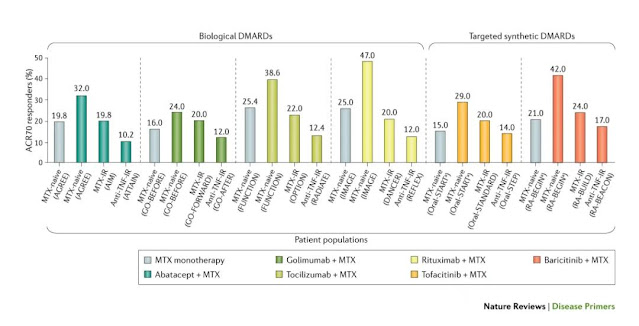
https://www.nature.com/articles/nrdp20181Treatment response measured by 70% improvement in the American College of Rheumatology (ACR) response criteria (ACR70) for methotrexate (MTX) and several biological and targeted synthetic DMARDs in three populations with rheumatoid arthritis (RA): individuals with RA who are MTX naive, who show an insufficient response (IR) to MTX or who experience failed anti-tumour necrosis factor (TNF) therapy (anti-TNF-IR).
'The number of methotrexate-naive patients who respond to methotrexate is within the same range of the number of those who had an inadequate response to methotrexate and were receiving biological DMARDs in addition to their methotrexate. However, the proportion of patients responding to methotrexate as a first DMARD plus the proportion of patients who respond to any biological DMARD after an insufficient response to methotrexate exceeds the proportion responding to biological DMARD plus methotrexate in methotrexate-naive patients.
This finding was also clearly illustrated in the OPTIMA trial. This trial further revealed that joint damage does not progress in individuals with early RA who receive methotrexate if stringent remission is achieved; even in non-responders, the progression of damage is minimal after 6 months when therapy is re-evaluated'
The OPTIMAL Trial has been shared below 👇🏻
Adjustment of therapy in rheumatoid arthritis on the basis of achievement of stable low disease activity with adalimumab plus methotrexate or methotrexate alone: the randomised controlled OPTIMA trial
This trial was done at 161 sites worldwide.
P- 1032 Patients with early (<1 year duration) rheumatoid arthritis were randomly selected
I - 515 Patients naive to methotrexate were randomly allocated to adalimumab (40 mg every other week) plus methotrexate (initiated at 7·5 mg/week, increased by 2·5 mg every 1-2 weeks to a maximum weekly dose of 20 mg by week 8)
C - 517 patients received placebo plus methotrexate for 26 weeks.
O-
Among 466 in patients receiving Methotrexate + Adalimumab 207 received low stable disease activity.
460 patients in the placebo plus methotrexate group, 112 achieved the stable low disease activity target
However, a higher proportion of patients treated with initial adalimumab plus methotrexate achieved the low disease activity target compared with those initially treated with methotrexate alone. Outcomes were much the same whether adalimumab was continued or withdrawn in patients who initially responded to adalimumab plus methotrexate.
https://pubmed.ncbi.nlm.nih.gov/24168956/
The American College of Rheumatology (ACR) improvement criteria are used to determine response to treatment; a treatment either reaches the level of improvement or no improvement.
Improvements in swollen and tender joint counts
Improvements compared with baseline values in three of the following five variables: patient global assessment, physician global assessment, patient pain assessment, physical function or quality of life score and acute-phase reactant levels (C-reactive protein or erythrocyte sedimentation rate)
An improvement of 20% (ACR20) is the minimal required response and implies that a 20% improvement in tender or swollen joint counts and a 20% improvement in at least three out of the five criteria is achieved. Improvements of 50% and 70% (ACR50 and ACR70 responses, respectively) are the corresponding reductions from baseline in the above variables.
B.
75 year old woman with post operative hepatitis following blood transfusion
Case details here: https://
1.What are your differentials for this patient and how would you evaluate?
https://www.google.com/search?q=Postop+hepatitis&prmd=inv&sxsrf=ALeKk02rxT3g3Efw4MktTL0hsuOAJettmg:1608200679331&source=lnms&tbm=isch&sa=X&ved=2ahUKEwjh5d-x5tTtAhXtzjgGHdxkC08Q_AUoAXoECAgQAQ&biw=412&bih=783&dpr=2.63#imgrc=Y9j2eirPppgY9M
Hepatitis is an inflammation of the liver with a variety of causes that include 5 hepatotropic viruses (HAV, HBV, HCV, HDV, HEV), nonhepatotropic viruses (cytomegalovirus, Epstein-Barr virus, herpes simplex virus, and varicella virus), infectious agents other than viruses (bacteria, fungi, parasites), drugs and toxic agents, autoimmune conditions, and metabolic disorders such as Wilson disease and α1-antitrypsin deficiency.
REGARDING ISCHAEMIC HEPATITIS
The liver receives about 25–30% of the cardiac output. Roughly 25% of the blood flow to the liver is oxygenated blood from the hepatic artery proper, which arises from the celiac trunk of the abdominal aorta. The remaining 75% consists of venous blood from the hepatic portal vein formed by the union of superior mesenteric and splenic veins.
During Intra operative procedure, 75 year old woman, wouldn't have been able to handle huge amount of blood loss plus certain anaesthesia drugs can lead to intraop hypotension leading to decreased hepatic blood flow.
Anesthesia alters hepatic blood flow by way of changing the hepatic perfusion pressure or splanchnic vascular resistance. This alteration is due to a variety of factors that include the effect of individual anesthetics, type of anesthesia, ventilation mode, and type of surgery.11 Most anesthetic agents that cause hypotension and decrease cardiac output also decrease the hepatic blood flow. During general anesthesia, as the splanchnic vascular resistance increases, the liver blood flow decreases. Application of positive end-expiratory pressure decreases the hepatic blood flow by increasing the hepatic portal venous pressure.
Isoflurane and sevoflurane largely preserve hepatic blood flow , while desflurane can reduce hepatic blood flow. Nitrous oxide at high concentrations may decrease hepatic blood flow secondary to a reduction in sympathetic innervation
Hepatocytes are responsible for producing the primary plasma binding proteins, albumin, and α1 acidic glycoprotein. Decreased protein binding leads to increased concentrations of unbound, active medications. Increased active medication concentrations, when coupled with diminished metabolic capacity, can lead to prolonged durations of action.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5467753/
REGARDING AUTOIMMUNE HEMOLYTIC ANEMIA
Occur 3–10 days after the transfusion of RBC products that appear to be serologically compatible. These reactions occur in patients who have been alloimmunized to minor RBC antigens during previous transfusions and/or pregnancies; pretransfusion testing fails to detect these alloantibodies due to their low titer. After reexposure to antigen-positive RBCs, an anamnestic response occurs, with a rapid rise in antibody titer.
4) 60 year woman with Uncontrolled sugars
http://manojkumar1008.
1. What is the problem representation of this patient?
60 year old woman who is a known case of Hypertension and diabetes since 2 years with a history of AKI and septic shock 1 1/2 years back presented with the complaints of chest pain since 4 days, Abdominal pain since 3 days.
She doesn’t seem to have tachypnea, tachycardia. And she is a febrile according to the details mentioned in the elog.
Her TLC is 18,000 c/cumm on the day of admission.
Doesn’t fit into SIRS criteria.
Her CUE shows 2 plus urinary sugars loss along with uncontrolled blood sugars.
She has indirect hyperbilirubinemia with a raised ALP and reduced serum albumin.
And a slight elevation in her Serum creatinine 1.5mg/dl - ?AKI
2. What are the factors contributing to her uncontrolled blood sugars?
Her Chest X-ray PA shows right upper lobe consolidation and the measurement of her average blood sugar levels over the past 3 months (HbA1C) is 8. Her blood sugars have already not been under control owing to her irregular use of OHA'S as it was mentioned in the history.
Her blood glucose shot through the roof even further after she developed Right lung pneumonia which inturn she would be more susceptible to because of poor blood glucose control.
3. What are the chest xray findings?
Her Chest X-ray PA shows right upper lobe consolidation
4. What do you think is the cause for her hypoalbuminaemia? How would you approach it?
Albumin being a negative phase reactant has reduced in this acute inflammatory condition. She otherwise doesn't seem to have renal failure neither liver failure.
Approach to hypoalbuminaemia
https://www.a4medicine.co.uk/hypoalbuminemia-low-albumin/#5. Comment on the treatment given along with each of their efficacies with supportive evidence.
Many antibiotics have been tried including Inj Monocef, Clarithromycin and Piptaz.
The effect of amoxicillin in lower respiratory tract infection (LRTI): A placebo controlled RCT in 16 primary care GRACE networks from 12 countries in Europe
P - 2054 patients presenting with uncomplicated acute cough (<4 weeks) as the main symptom were randomised to amoxicillin 1g three times a day or placebo for 7 days.
In the first 4 days after seeing the doctor (placebo mean 1.69, antibiotic 1.62; difference -0.07 (-0.18 to 0.06)), and no significant difference in the proportion with moderately bad or worse symptoms at 7 days (47% vs 40% respectively, p=0.07). Among the subgroup of patients aged 60 or over there was no evidence of selective benefit. 5% more patients in the antibiotic group compared with the placebo group developed nausea, rash or diarrhoea
O- Antibiotics are very unlikely to provide meaningful symptomatic benefit in LRTI for most patients, and any benefit is likely to be similar to the magnitude of harm
https://erj.ersjournals.com/content/38/Suppl_55/4509
5) 56 year old man with Decompensated liver disease
Case report here: https://appalaaishwaryareddy.
1. What is the anatomical and pathological localization of the problem?
3. What is the pathogenesis of the illness due to Hepatitis B?
6) 58 year old man with Dementia
Case report details: http://
1. What is the problem representation of this patient?
58 year old man with Slurring of speech since 6 months
Drooling of saliva and food from the mouth since 6 months
Urinary incontinence since 6 months
Forgetfulness since 3 months
Dysphagia to both solids and liquids since 10 days
2. How would you evaluate further this patient with Dementia?
https://www.aafp.org/afp/2018/0315/p398.html
https://www.aafp.org/afp/2018/0315/p398.html
Yes
Dementia is common after stroke but we know little of the mechanisms or whether the risk varies with stroke subtype.
Stroke risk factors, amounts and regions of the brain affected, and suggested stroke mechanisms all vary with stroke subtype, and could influence the risk of cognitive impairment after stroke. For example, as cortical ischaemic strokes often affect a large area of brain, they may carry a higher risk of cognitive impairment than the smaller, less neurologically severe, lacunar strokes. Alternatively, lacunar strokes may carry a higher risk of cognitive impairment than would be expected on the basis of the lacunar infarct alone as they are part of the spectrum of cerebral small vessel disease (SVD). SVD, which affects the brain diffusely and is the commonest vascular cause of cognitive impairment, could be unmasked by a new lacunar stroke.
https://jnnp.bmj.com/content/84/8/893
4. What is the likely pathogenesis of this patient's dementia?
5. Are you aware of pharmacological and non pharmacological interventions to treat such a patient and what are their known efficacies based on RCT evidence?
Randomized, placebo-controlled, clinical trial of donepezil in vascular dementia
This international, multicenter, 24-week trial was conducted from March 2003 to August 2005.
P - 974 Patients with probable or possible VaD were randomized 2:1 to receive donepezil 5 mg/d or placebo
I - Donepezil 5mg/d
C - Placebo
O - Patients with hippocampal atrophy who were treated with donepezil demonstrated stable cognition versus a decline in the placebo-treated group; in those without atrophy, cognition improved with donepezil versus relative stability with placebo.
Patients treated with donepezil 5 mg/d demonstrated significant improvement in cognitive, but not global, function.
https://pubmed.ncbi.nlm.nih.gov/20395618/
7) 22 year old man with seizures
Case report here http://geethagugloth.
1. What is the problem representation of this patient ? What is the anatomic and pathologic localization in view of the clinical and radiological findings?
22 year old man with complaints of headache since 2 months and involuntary stiffness of bilateral upper and lower limbs since 1 week along with Loss of consciousness.
Anatomical localisation - Brain
Involving both the upper limbs and lower limbs
Could be due to multiple infarcts
Ring enhancing lesions as he is RVD positive
Radiologically
Shows ring enhancing lesions
2. What the your differentials to his ring enhancing lesions?
Cerebral abscess
Tuberculoma
Neurocysticercosis
Metastasis
Glioblastoma
Subacute infarct/haemorrhage/contusion
Demyelination (incomplete ring)
Tumefactive demyelinating lesion (incomplete ring)
Radiation necrosis
Postoperative change
Lymphoma - in an immunocompromised patient
Leukaemia
Thrombosed aneurysm
Necrotising leukoencephalopathy after methotrexate
A helpful mnemonic is MAGIC DR
https://radiopaedia.org/articles/cerebral-ring-enhancing-lesions
3. What is "immune reconstitution inflammatory syndrome IRIS and how was this patient's treatment modified to avoid the possibility of his developing it?
A paradoxical clinical worsening of a known condition or the appearance of a new condition after initiating antiretroviral therapy in HIV-infected patients is defined as immune reconstitution inflammatory syndrome.
Despite numerous descriptions of the manifestations of IRIS, its pathogenesis remains largely speculative. Current theories concerning the pathogenesis of the syndrome involve a combination of
1. Antigenic burden
2. degree of immune restoration following
3. Host genetic susceptibility.
https://www.mdpi.com/life/life-10-00262/article_deploy/html/images/life-10-00262-g001.png
Major criteria
Atypical presentation of “opportunistic infections (OI) or tumors” in patients responding to antiretroviral therapy.
Decrease in plasma HIV RNA level by at least 1 log10copies/mL.
Minor criteria
Increased blood CD4+ T-cell count after HAART.
Increase in immune response specific to the relevant pathogen, e.g. DTH response to mycobacterial antigens.
Spontaneous resolution of disease without specific antimicrobial therapy or tumor chemotherapy with continuation of antiretroviral therapy.
BHIVA has issued guidelines for starting the TB treatment with HAART. If CD4+ count is less than 100 cells/μl, both anti-tuberculosis drugs and HAART can be started together. If CD4+ cells are in the range of 100-200; HAART is started 2 months after starting TB treatment. If the CD4+ cells are above 200, HAART is started 6 months after completing TB treatment.
https://www.mdpi.com/2075-1729/10/11/262/htm
https://encrypted-tbn0.gstatic.com/images?q=tbn:ANd9GcRWT7mETAJI7Y8GmY0_MaTdRWszlQ6OhYpo5Q&usqp=CAU
8) Please mention your individual learning experiences from this month.
November 29 was my duty day. We had 3 admissions in our unit.
One was that of a 32 year old woman with progressive blindness and Polyuria since 2 years. She was diagnosed to be HCV positive a week back.
Along with a 75 year old man with dengue NS1 positive and
A 55 year old man with Recurrent episodes of right focal seizures and right hemiparesis with left fronto parietal region infarct and Nstemi were admitted by us in our unit.
30th the following day, which was a Sunday usually goes by following up reports of the cases, filling up Pending case sheets and of course examining cases
31st went by doing rounds for our patients, reading up regarding our admitted cases and going through elog links created.
Me and my junior examined our 55 year old man with Recurrent Focal Seizures, we did all the lobar function tests and discussed with the interns regarding the motor and premotor cortex.
We also did a 2decho for him to look for any RWMA but there was nothing as such
By then he was started on Inj levipil 1gm BD but we had to increase the dose as his seizures episodes weren't coming down.
For the 32 year old woman, we put her on Tab Glimi M1 BD and were monitoring her blood sugars
75 year man with dengue fever improved overnight so did his platelet counts
1st went by reading up about our cases.
Reviewed literature regarding use of Enoxaparin vs Heparin in Nstemi and shared the article on our respective groups. Started our patient on Inj Enoxaparin.
Read the causes for blindness in young as our patient was only 32years with a history of trauma 3 years back. But after discussions decided that diabetes was probably the cause for her progressive blindness.
2nd December - our patient continued to have focal seizures for which we started him on Carbamazepine
3rd December - Tuesday following rounds
And read about the differences between VPCs and APCs and fasicular blocks as LAFB was present for our 55 year male patient
4th December - attended rounds and studied about Stroke
5th December - Looked up at the efficacy of Sodium valporate vs levipil as discussed and presented in the previous days 2-4pm session
6th December - Prepared discharge notes for my patients. Did 2decho for patients who came for cardiology opinion.
7th December - was my duty day.
Admitted 3 cases.
66 year old man with hypertensive emergency with Left heart failure, PVD, known case of type 2 DM and? Recurrent subendocardial ischaemia in anteroseptal leads
35 year old man with AKI
8th December - Examining the admitted cases, following up reports, discussing treatment regimens with the team
Started our 65 year old hypertensive emergency case on Ntg drip
And started him on a preload and afterload reducing agents
9th December - slowly tapered off Ntg
10th - Our 35 year man with AKI was started up on haemodialysis
11th - Our 65 year old patient got symptomaticaly better. Took cardiology opinion.
12th - Studied about PVD and AKI.
13th - Attended rounds and studied about heart failure
14th was my duty day and admitted 4 cases
45 year man with Heart failure with severe TR and PAH, congestive hepatopathy and AKI
65 year woman with Parkinson's disease
40 year man with Acute Pancreatitis
22 year old boy with Cerebral palsy and recurrent seizures
15th - Following up case reports and examining our patients.
Our 45 year man had a palpable S2, read about TR
Read about Parkinson's disease
16th - Performed 2decho for our in patients.
Our 65 year woman had severe AS with ASD
17th - Our 45 year man with Heart failure, his TR and PAH reduced after thiamine doses and diuretics
Neurology opinion for our cases were taken and he was in the opinion that the weakness in our 22year boy with CP was due to phenytoin toxicity which we already withheld and started on sodium valporate
































Comments
Post a Comment