Bimonthly internal assessment for the month of March 2021
"This is my submission for the Bimonthly internal assessment for the month of March."
Most of the information here have been collected from different reference sites, the links to which have been mentioned. The points copy pasted have been put in quotes.
The questions to the cases being discussed can be viewed from the link below 👇
https://
Case 1. https://ashakiran923.blogspot.
a). What is the problem representation of this patient and what is the anatomical localization for his current problem based on the clinical findings?How specific is his dilated superficial Abdominal vein in making diagnosis?
1. The problem representation:
A 60 year old man who was a smoker and alcoholic, has been on conservative treatment for CKD presented with fever and dyspnea since 15 days
2. Anatomical localization:
Here, from the history of fever since 15 days and dyspnea which initially was only on exertion and which later on progressed to at rest, he had no complaints of orthopnea, bendopnea, chest pain or palpitations
Along with facial puffiness
This picture could suggest the possibilities of :
Renal failure
Heart failure
Liver pathology
As the heart failure symptoms have been ruled out, from the history it suggests probably the presence of a renal or a liver pathology.
And the investigations shows a picture of urinary tract infection on an already present chronic kidney disease
Along with hypoalbuminaemia, raised alkaline phosphatase and pancytopenia suggesting a liver failure.
So this gives an anatomical location of
UTI on Chronic kidney disease
Liver failure.
2. And with the presence of dilated abdominal veins suggests a liver pathology.
Dilated abdominal vein is important in differentiation cirrhosis from vena caval obstruction. In patients with dilated abdominal wall veins due to cirrhosis, the direction of blood flow is away from the umbilicus (radiating like a star from the umbilicus), whereas in vena caval obstruction, the direction of blood flow is either completely above downward (superior venacaval obstruction) or completely below upward (inferior venacaval obstruction).
b) What is the etiology of the current problem and how would you as a member of the treating team arrive at a diagnosis? What is the cause of his hypoalbuminemia?Why is the SAAG low?
B.
1. Etiology to the current problems:
Fever is because of urinary tract infection
Dyspnea and facial puffiness is because of AKI on already pre existing kidney failure
AKI on CKD
The patient also gives a history of being diagnosed outside of renal failure around 3 months back and also has received 1 hemodialysis session in another hospital and has been on conservative management since then.
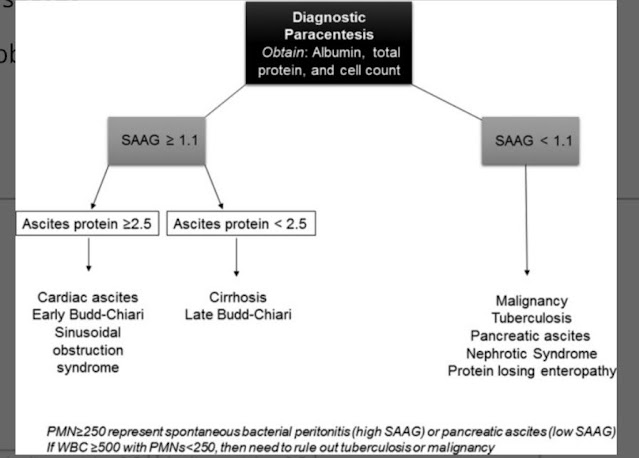
2. Low SAAG ascites (<1.1 g/dL) is usually caused by peritoneal malignancies, chronic peritoneal infection (i.e., mycobacterium tuberculosis), and nephrotic syndrome. Low serum oncotic pressure can also cause low SAAG ascites. Testing for nephrotic syndrome and protein‐losing enteropathy should be performed in patients with low SAAG ascites and a suspicion of either one of these conditions.
In patients with cirrhotic ascites, the presence of more than 250 polymorphonuclear cells (PMNs) is consistent with spontaneous bacterial peritonitis. The PMN count can also be elevated in pancreatic ascites, but the SAAG in these patients will be less than 1.1 g/dL.
However in this patient, the ascitic cell count doesn’t give a picture of peritonitis.
3. The cause for his hypoalbuminaemia
This beautiful diagram shows the synthesis, distribution and elimination of albumin in the human body.
The cause for his hypoalbuminaemia is because of the liver failure.
The urine doesn’t show significant albuminuria.
The hypoalbuminaemia could also be because it acts a negative phase reactant in infectious conditions.
c)Will PT,INR derangement preceed hypoalbuminemia in liver dysfunction??Share reference articles if any!
Liver disease results in complex alterations of all 3 phases of hemostasis: primary hemostasis, coagulation, and fibrinolysis. Liver is the site of synthesis of fibrinogen and factors II, V, VII, IX, X, XI, XII.
In acute liver failure, plasma concentration of coagulation factors first those with the shortest half life, factor V and VII (12 h and 4-6 h respectively), and factors II, VII and X subsequently. Factor VIII, together with vWf is usually elevated.
However the half life of albumin is around 20 days, which points towards that the coagulation profile will be first deranged prior to hypoalbuminaemia.
d)What is the etiology of his fever and pancytopenia?
The cause for his fever can be attributed to his Urinary tract infection and the cause for his pancytopenia is because of liver failure.
e)Can there be conditions with severe hypoalbuminemia but no pedal edema? Can one have hereditary analbuminemia and yet have minimal edema? Please go this article https://www.frontiersin.org/articles/10.3389/fgene.2019.00336/ full and answer the question.
1. As an acute phase reactant:
The liver responds to infections and inflammations by producing a large number of APRs. At the same time, the production of a number of other proteins is reduced, these are therefore referred to as “negative” APPs. Negative APPs are albumin, transferring, transthyretin, transcortin, and retinol-binding protein.
2. Protein-losing enteropathy is a syndrome where there is an excess loss of proteins in the gastrointestinal tract.
3. Nutritional Hypoalbuminaemia
They have low serum albumin levels due to a decreased supply of amino acids to the liver as well as other nutritional deficiencies.
Yes hereditary hypoalbuminaemia can have minimal edema. According to this article,
‘Clinically, in addition to the low level of albumin, the patients almost always have hyperlipidemia, but they usually also have mild oedema, reduced blood pressure and fatigue.'
f) What is the efficacy of each of the drugs listed in his current treatment plan
1. NITROFURANTOIN:
Randomised controlled trial of nitrofurantoin versus placebo in the treatment of uncomplicated urinary tract infection in adult women
P - 78 patients with UTI
I - 40 patients were randomised to receive nitrofurantoin 100 mg four times daily for three days.
C - 38 patients received Placebo
O - The result for combined symptomatic improvement and cure after three days was 27/35 in the nitrofurantoin group and 19/35 in the placebo group. After seven days, combined improvement and cure was observed in 30/34 and 17/33 respectively.
After seven days the bacteriological cure rate was 17/23 in the intervention group and 9/22 in the placebo group.
women with bacteriologically proven UTI, nitrofurantoin was significantly more effective than placebo in achieving bacteriological cure and symptomatic relief in just three days; this was still present after seven days. In patients with clinically suspected UTI the symptomatic effect was statistically significant after.
2. TAMSULOSIN:
Randomized, double-blind, placebo-controlled trial conducted at 95 urology clinics in the United States involving men 40 years and above
I - Patients were randomly assigned to receive placebo (n = 222), 4 mg of tolterodine ER (n = 217), 0.4 mg of tamsulosin (n = 215), or both tolterodine ER plus tamsulosin (n = 225) for 12 weeks.
C - total of 172 men (80%) receiving tolterodine ER plus tamsulosin reported treatment benefit by week 12 compared with 132 patients (62%) receiving placebo (P<.001), 146 (71%) receiving tamsulosin, or 135 (65%) receiving tolterodine. Patients receiving tolterodine ER plus tamsulosin compared with placebo experienced significant reductions in urgency urinary incontinence, urgency episodes without incontinence, micturitions per 24 hours, and micturitions per night.
O- These results suggest that treatment with tolterodine ER plus tamsulosin for 12 weeks provides benefit for men with moderate to severe lower urinary tract symptoms including overactive bladder.
2nd Case:
45year old female with abdominal distension
a). What is the problem representation of this patient and what is the anatomical localization for her current problem based on the clinical findings?
45 year old woman known case of diabetic since 6 months, presented with
Abdominal distension since 2 years
Bilateral pedal edema since 2 months
Dyspnea since 2 months
Lower back pain since 2 months
Her Anatomical localization Refractory Ascites with right sided pleural effusion
On clinical examination - There is fullness of flanks along with presence of fluid thrill.
Dull note on percussion and decreased breath sounds on the right side.
b) What is the etiology of her refractory ascites and pleural effusion? and how would you as a member of the treating team arrive at a diagnosis?
Refractory ascites is defined as ascites that does not recede or that recurs shortly after therapeutic paracentesis, despite sodium restriction and diuretic treatment.
CAUSES OF REFRACTORY ASCITIS:
1.Non compliance to treatment
2.Renal failure
3.Tumor hepatoma
4.spotaneous bacterial peritonitis
5.Portal vein thrombosis
6.NSAIDS
7.Infection
8.GI Bleeding
ARRIVING AT THE DIAGNOSIS OF REFRACTORY ASCITES
c) Approach to a patient with ascites?Clinically is there any way to differentiate pre hepatic, post hepatic and hepatic causes?
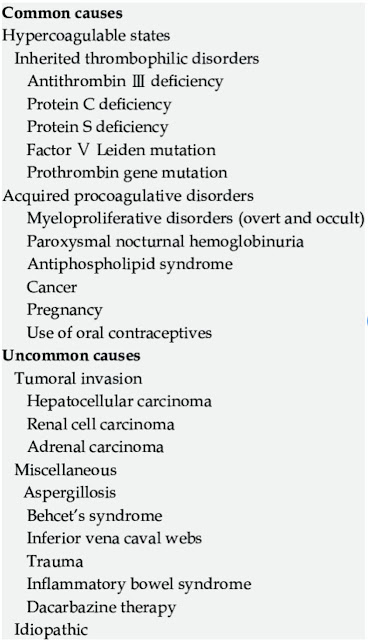
d)Causes of budd chiari syndrome?Why did the patient undergo bone biopsy?
Bone biopsy was done from posterior iliac crest to evaluate osteolytic lesions in the pelvis, ribs and vertebrae to rule out sarcoidosis, metastasis.
d) Management strategies for refractory ascites and Budd chiari syndrome? Share the potential advantages and disadvantages of Peritoneal dialysis catheter placement in
refractory ascites?
Unlike haemodialysis, an advantage of peritoneal dialysis is that regular visits to a dialysis unit are not required, and it can be carried out at home.
Another major disadvantage of peritoneal dialysis is that you're at risk of developing peritonitis.
In rare cases, your peritoneum may gradually become thickened and scarred.
Another drawback of peritoneal dialysis is that the dialysis fluid used can cause a reduction in protein levels.
Advatanges of peritoneal dialysis:
Better cardiovascular stability
e) What is the efficacy of each of the drugs listed in his current treatment plan
To compare the efficacy of three commonly used diuretic regimens in the treatment of ascites, we randomized 90 patients to three treatment groups: Sequential Spironolactone (spironolactone followed by furosemide if necessary), Combination (spironolactone and furosemide in combination), and Furosemide (furosemide given alone).
Diuretics were begun at a low dose by mouth and the dosage increased until a 0.4-0.8 kg daily diuresis was achieved.
To do so was far more difficult with furosemide alone, which required repetitious upward adjustments in dosage and massive KCl supplements. The incidence of encephalopathy, hepatorenal syndrome, and marked electrolyte abnormalities was similar for the three treatment groups except that severe hyperkalemia was more frequent on combination therapy. We conclude that diuresis should be initiated with one of the two spironolactone regimens and not with furosemide as the sole agent.
f)What is the current outcome?and what could be the etiology of her current outcome?
The patient was declared dead on March 14th
The cause was probably due to pulmonary embolism
Case 3:
55year old male with SOB and abdominal distension,orthopnea
https://jayanth1802.blogspot.com/2021/02/55-year-old-farmer-with-sob-abdominal.html?m=1
a). What is the problem representation of this patient and what is the anatomical localization for his current problem based on the clinical findings?
A 55 year old man, alcoholic and smoker, a known case of COPD presented with
Dyspnea at rest since 4 days
Abdominal distension along with scrotal swelling since 1 week
Reduced urine output, facial puffiness
The anatomical localization is in the heart as it's consistent with the symptoms and the cvs examination reveled thrills in the left and right paraphernalia areas along with visible pulsations.
Pansystolic murmur was heard in Mitral and tricuspid areas.
b) What is the etiology of his ascites? and how would you as a member of the treating team arrive at a diagnosis?Chart out the sequence of events!
SAAG is 1.9
Which suggests a high SAAG indicating portal hypertension.
However this picture of High SAAG (1.9) with ascitic protein of 2.1g/dl is seen in Cirrhosis and Late Budd Chairi. However, this patients usg abdomen shows no picture of Cirrhosis.
Chronic smoker and alcoholic -------> COPD --------->
Cor Pulmonale -------> Congestive Hepatopathy
c)What is the efficacy of each of the drugs listed in his treatment plan?
1. 'Bronchodilator efficacy of salbutamol (200 micrograms), salmeterol (50 micrograms) and ipratropium bromide (40 micrograms) aerosols has been compared in 16 patients with stable chronic obstructive pulmonary disease (COPD) using a double-blind placebo controlled cross-over design.
When absolute changes in FEV1 were used as the response criterion, efficacy of the three drugs was significantly better than placebo (P < 0.05).
The onset of bronchodilatation after ipratropium bromide was slower than after salbutamol, but ipratropium induced more and longer-lasting bronchodilatation than the adrenergic drug. Salmeterol was slower but its duration was longer than salbutamol. The onset of the effect of salmeterol was slower than ipratropium bromide, but salmeterol showed, on average, superior bronchodilator efficacy compared with the anticholinergic agent, sustaining bronchodilation longer than ipratropium bromide (responses to salmeterol were significantly (P < 0.05) greater than those to ipratropium bromide from 4-12 h time period, but from 15 min to 1 h time periods response to ipratropium bromide exceeded salmeterol). The mean FEV1 area under the curve was significantly (P < 0.05) larger after salmeterol when compared to ipratropium bromide and salbutamol. Moreover, the mean FEV1 area under the curve after ipratropium bromide was significantly.
O- Salmeterol compares favourably with ipratropium bromide in terms of effects on lung function at clinically recommended doses because it has a longer duration of action than ipratropium bromide. The longer dosing intervals, which may enhance compliance, encourage its administration in patients with COPD.'
2. This study suggests that a low-sodium and fluid-restricted diet, compared with a non-restricted diet, for patients hospitalized with acute decompensated heart failure does not expedite weight loss or decrease congestion.
This is a randomized controlled trial
Patients in the intervention group (n = 38) had a fluid intake of 800 mL per day and a sodium intake of 800 mg per day until discharge or hospital day 7, whichever came first.
Patients in the control group (n = 37) received liberal fluids and sodium (at least 2.5 L per day and 3 to 5 g per day, respectively).
Patients in both groups lost approximately 4.5 kg (10 lb) of body weight during this time. The restricted group had significantly greater perceived thirst than the control group. At 30-day follow-up, patients in the restricted group were noted to be slightly more congested, with a clinical congestion score 2.4 points higher than the control group, but there was no difference in 30-day readmission rates between the groups. Given the small sample size, this study was likely underpowered to detect such a difference if it exists.
d) What are his current outcomes?
The patient was declared dead due to a cardiopulmonary arrest as a result of
acute exacerbation of COPD with cor pulmonale and Severe PAH
c) Please evaluate this randomized controlled trial on different techniques at ascitic tap here: https://pubmed.ncbi.nlm.nih.
QUESTION 4
4)Please go through the thesis presentation below and answer the questions below by also discussing them with the presenter
a)What was the research question in the above thesis presentation?
To evaluate the etiology of ascites through SAAG
b) What was the researcher's hypothesis?
According to the researcher, SAAG is better for etiological diagnosis for ascites when compared to ascitic fluid total protein
c)What is the current available sensitivity and specificity of SAAG in diagnosis of etiology of ascites
The aim of this study was to define a new reasonable threshold of SAAG in Chinese ascitic patients.
Adult patients with ascites admitted to the Shanghai Changzheng Hospital from Jan 2004 to Jun 2010 were retrospectively analyzed. The diagnostic criteria for cirrhotic ascites are clinical manifestations, radiological features and esophageal-gastric varicosis, or histopathology.
The mean value of SAAG in portal-hypertension-related ascites was significantly higher than that in the non-portal-hypertension-related ascites (21.15 ± 4.38 g/L vs 7.48 ± 3.64 g/L, P = 0.002). The SAAG cut-off value under 12.50 g/L predicted portal hypertension ascites with the sensitivity of 99.20%, specificity of 95.10% and accuracy of 97.65%.
SAAG is useful to distinguish portal-hypertension-related ascites and non-portal-hypertension-related ascites, and 12.50 g/L might present as a more reasonable threshold in Chinese ascitic patients.
5) Journal club questions on Ascites theme
a) Please identify the study design and outcomes in the article linked here https://www.ncbi.nlm.nih.
The study design here is a Prospective type of study
A total of 52 patients were included in this study from November 1, 2018 to March 30, 2019.
Chronic liver disease (CLD) was the major cause of ascites in this study in 24 (46.2%) patients. The other main causes of ascites were heart failure from various causes (19.2%), tuberculosis and hepatosplenic schistosomiasis contributing to 11.5% each and chronic kidney disease (5.8%). Five (20.8%) CLD patients had spontaneous bacterial peritonitis as a complication. Five (20.8%) and 4 (16.7%) CLD patients had hepatocellular carcinoma and hepatic encephalopathy as complications, respectively. Nine (17.3%) patients had variceal bleeding; six of the patients were diagnosed to have CLD while the remaining patients were having hepatosplenic schistosomiasis.
b) Please download the CASP diagnostic study checklist here https://casp-uk.net/casp-
THANK YOU :)




















Comments
Post a Comment